Medical lasers continue to gain adoption and utilization in ORs across the country, providing exciting new options for more precise and less invasive treatments. Yet, inconsistent safety practices present heightened risks to both patients and staff.

Richard Gama, Director of Laser Safety at Agiliti, talked with the hosts of First Case Podcast to discuss why medical lasers present such unique risks and challenges, what hospitals commonly get wrong when it comes to laser safety and how proper laser safety creates a unique “synergy between patient and employee safety.”
Listen to the full episode, Protection and Prevention: Understanding Laser Safety in the Operating Room, here:
Below are a few key insights from the conversation.
Medical Lasers Present Unique (and Overlooked) Health and Safety Risks
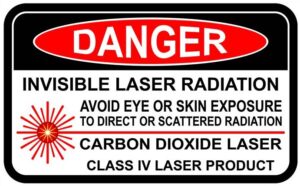
Medical lasers are categorized by ANSI and the FDA into four major hazard classes, with the highest risk category (Class IV) presenting the risk of serious injury if used improperly. Lasers in this category are often the most high-powered and use non-ionizing radiation.
While many people understand that ionizing radiation is very hazardous to their health, they might not know or understand that the hazards of laser energy are also a very serious concern in terms of safety.
The biggest safety risk is eye injury, but lasers can also cause skin burns — for both patients and staff. Medical lasers also present a serious fire risk because they can easily ignite combustible materials.
Laser Smoke Plumes Have Pathological Risks
Perhaps the most overlooked risk of medical lasers comes from the smoke plumes emitted during procedures. These plumes can potentially contain intact viral particles that are thought to be able to transmit different pathologies, such as HPV.
Nevertheless, compliance issues persist around smoke evacuation requirements for surgical laser procedures. You cannot rely on a high filtration breathing mask or standard wall suction in the OR as your first line of defense. What is your best defense? A smoke evacuation system — either a mobile unit or one that’s installed in the OR in the proper position. However, many times they are intentionally not used because of the noise they generate.
Note: Ten states have enacted legislation mandating the use of smoke evacuation equipment: Connecticut, Georgia, Kentucky, Illinois, Iowa, New Jersey, Oregon, Tennessee, Utah and New York.
Debunking Misinformation Around the Laser Safety Officer Role
Gama and the First Case hosts went deep on “misinformation” about the medical laser safety officer (MLSO) role. Some mistakenly believe the MLSO has to be a medical doctor (it doesn’t), or that ORs can fully rely on a third-party laser vendor to act as the MLSO during use of laser systems.
The most common mistake hospitals make with MLSOs is trying to add the responsibility to someone else with competing responsibilities, or to someone who does not have the knowledge, background or experience necessary to fill this role.
Three Steps Hospitals and OR Teams Can Take to Improve Laser Safety
In addition to their discussion around the MLSO, Gama also focused on three things hospitals and OR teams should be doing now to address laser safety needs:
- Provide regular training and education: A top-down culture of safety in the OR is critical to supporting and reinforcing training. Some staff may not understand the risks they’re facing and how to identify disinformation.
- Laser safety trainings should be laser-specific, wavelength-specific, device-specific and application-specific. This is important because all lasers have unique risk factors and have different best practices and safety protocols that need to be understood.
- While staffing shortages, cost and availability of training resources can hinder the ability to provide training, there are external education and training resources available to help staff keep informed on industry changes and perform their jobs to the highest standard.
- Set their own safety standards: Hospitals need to define their laser safety standards, as well as the metrics or KPIs they will use to monitor compliance. Just as importantly, hospitals need to ensure their internal policies are based on the most current regulatory standards.
- Enforce laser safety policies: It’s not enough to have a policy. You also have to enforce the policies if you want to create a culture of trust and safety for staff and patients.
Dive deeper and listen to the full episode above or listen here to learn more about these topics, including additional tips on how you can build and sustain a modern medical laser safety program that’s agile – and responsive – to evolving use cases and changing regulations.
More information about the First Case Podcast can be found at firstcasemedia.com and on Facebook and LinkedIn.
You can subscribe and listen to the First Case operating room podcast on your favorite podcast app:
- Apple Podcasts -> https://apple.co/3beyevM
- Google Podcasts -> http://bit.ly/2NyVGtV
- Amazon Podcasts -> https://amzn.to/3rMjURj
- Spotify -> https://spoti.fi/3rUtTUq
- Stitcher -> https://lnkd.in/e_JgNsb
- iHeartRadio -> http://ihr.fm/3dbxOYi
Access additional resources around medical laser safety practices in the operating room here:










