Sterile processing technicians rarely interact with patients, view surgeries or hear about procedure outcomes – unless something goes wrong. And things do occasionally go wrong – from delayed cases to malfunctioning equipment (like endoscopes) to infection risks. Gaps in processes, whether in the Sterile Processing Department (SPD) or in the point of use cleaning practices of the operating room – or both – can have a detrimental impact on patient care.

Michael Matthews, MBA, CLSSGB, Director of Customer Training and Education at Agiliti, joined the hosts of First Case Podcast to discuss the relationship between SPD and OR and best practices for the cleaning and the sterilization of surgical instruments to minimize preventable damage, avoid errors and save on repair costs.
The full episode, Whose Job is it Anyway? Recognizing the Importance of Instrument Care in the OR is available here – or listen below.
Below are six key insights from their conversation.
Insight #1: Don’t Use Saline When Cleaning Surgical Instruments
Saline is used in almost all surgeries. But leaving saline on surgical instruments can make cleaning them harder and can cause damage. What makes saline not safe for surgical instruments?
- Stainless steel surgical instruments are water-resistant and strong. Think of stainless steel instruments like Superman. But their Kryptonite is salt – and saline is a mixture of salt and water.
- Operating rooms typically are cool and have very low humidity, which can cause the water part of saline to evaporate quickly – leaving behind the Kryptonite – salt, which can cause corrosion.
- Soaking instruments in a saline bath is far worse than wiping with saline – it’s quite literally a salt bath.
Instead of saline, use sterile water to pre-clean surgical instruments.
Insight #2: Use Enzymatic Spray to Break Down Blood on Instruments
After a case is completed, OR teams should begin the cleaning process by spraying instruments with an approved enzymatic pretreatment. Enzymatic spray breaks down certain materials such as proteins, lipids and starches found in blood and bodily fluids and prevents them from drying on instruments.
- Dried blood on instruments makes them difficult to clean, increasing the time required to decontaminate the instruments properly and the likelihood of bioburden making it through reprocessing (potentially contaminating a future case).
- However, enzymatics will not prevent the salt from saline from damaging the stainless steel and is not a substitute for proper cleaning practices during the case.
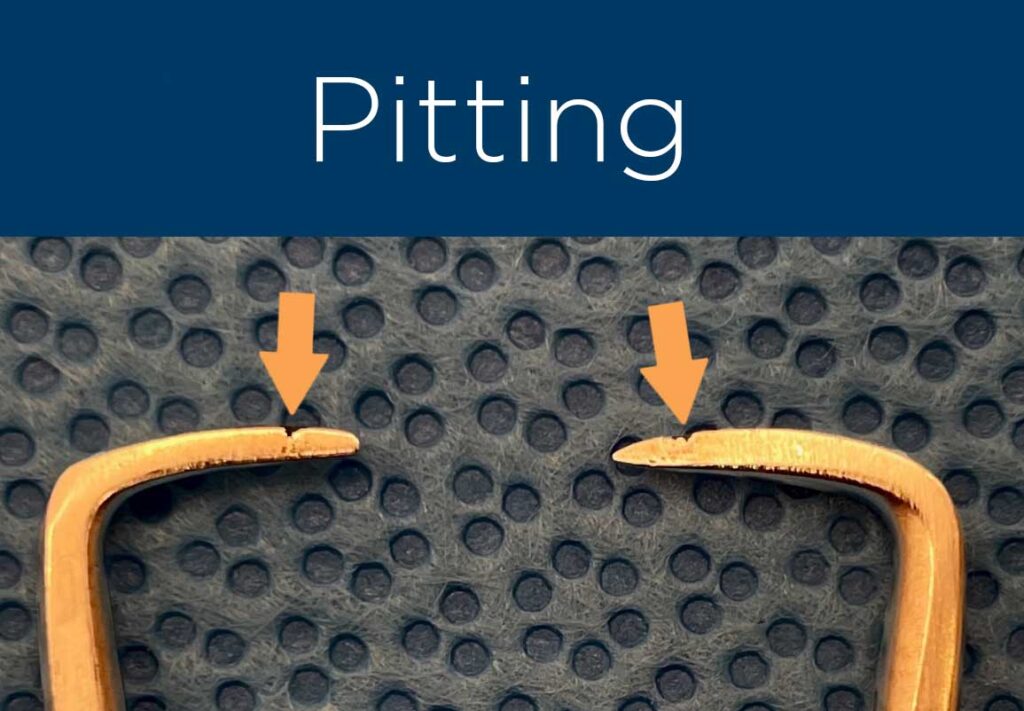
Insight #3: Pitting is Problematic – Learn How to Spot Pitting to Avoid this Costly Damage
Pitting is a highly localized corrosion that appears as black dots (pits) on the instruments surface. Pitting can sometimes be microscopic, and most OR staff are not equipped (or trained) to identify pitting or discoloration from stains. SPD should be the stop gap to detect signs of pitting and ensure instruments are safe for patient use.
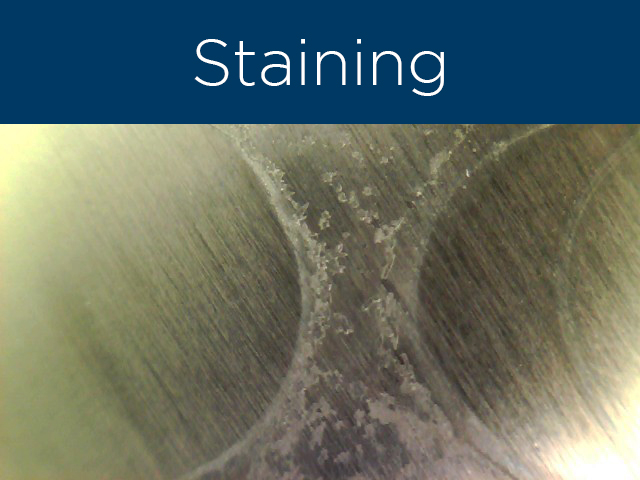
Insight #4: Instrument Stains are Gaining Industry Attention
Inspections from The Joint Commission are increasingly focused on surgical instrument conditions. Inspectors are looking for the root cause of defective instruments — related both to prevention and errors. Be aware that The Joint Commission might focus on this during your next inspection, so make sure you have a defined process that shows steps to address common issues related to instrument staining.
Insight #5a: Water Quality Can be a Root Cause of Staining
Getting to the root cause of stains can be difficult. However, the most likely cause is poor water quality or lack of preventive maintenance. There are three ways water quality can impact the instruments coming out of sterile processing:
- Decontamination water (from sinks and washers): Many hospitals use reverse osmosis water in the final rinse of the washers to help control the fluctuations in water quality. As water dries on instruments, it evaporates and leaves behind minerals that build up over repeated washings in the form of water staining. The amount of mineral content in the water will affect how quickly the stain becomes visible and creates problems in both the appearance and functionality of the instruments.
- Autoclave steam: Most hospitals use the steam coming from their facility’s boiler system, which does not follow the parameters recommended for reprocessing stainless steel There are many instances where the facility management team may be adding a chemical to their boiler for their own purposes which can cause staining to instruments.
- External factors: Outside forces like nearby municipal construction projects can impact water quality and can also be the culprit of sudden staining.
Insight #5b: Elevated Water Quality Requirements are Coming Soon
A new Association for the Advancement of Medical Instrumentation (AAMI) standard is coming out soon (ST108) which heightens requirements for water used in device reprocessing, including:
- Municipal water supply likely won’t qualify under the new standard.
- The standard will apply to the quality of water fed into steam lines and final rinse.
Insight #6: Taking Care of Instruments is Taking Care of Patients
Surgical instruments are critical to safe patient care. If surgical instruments are contaminated or damaged, it can lead to an adverse outcome on the patient. Fostering a relationship between the OR and SPD can be a powerful way to ensure both departments meet their goals around patient safety.
- Create a two-way dialogue between SPD and the OR to foster collaboration and create trust between the departments.
- Surgical staff should go down to SPD and learn about the sterilization processes.
- Give SPD staff opportunities to sit in on surgical cases so they can better understand the needs of the OR and the impact instrument quality and availability have on surgeries.
- Surgical staff and SPD leaders should tell sterile processing techs and staff when things go right – and about what went right and why – to create a culture that celebrates success instead of only pointing out when there are issues.

About Michael Matthews
Michael Mathews comes from the world of sterile processing. He is a Certified Registered Central Service Technician, a Certified Instrument Specialist, Certified in Healthcare Leadership, a Lean Six Sigma Greenbelt and is a well-known innovator and expert in the sterile processing field. Matthews has published articles in Infection Control Today and Becker’s Hospital Review as well as several LinkedIn articles for the Sterile Processing community. For the episode, Mathews was joined by the hosts Paul Wafer (BS, MBA, RN), Melanie Berry (BSN, RN, CNOR, CCSM) and Justin Pullen (Co-Founder and Chief Executive Officer at Beyond Clean). More information about the First Case Podcast can be found at firstcasemedia.com and on Facebook and LinkedIn.
You can listen to First Case podcasts on a variety of apps:
- Apple Podcasts -> https://apple.co/3beyevM
- Google Podcasts -> http://bit.ly/2NyVGtV
- Amazon Podcasts -> https://amzn.to/3rMjURj
- Spotify -> https://spoti.fi/3rUtTUq
- Stitcher -> https://lnkd.in/e_JgNsb
- iHeartRadio -> http://ihr.fm/3dbxOYi
Interested in learning more?
These insights just scratch the surface on the proper care and handling of surgical instruments. To go more in-depth and access continuing education and pre-certification resources, visit agilitihealth.com/clinical-support/education or contact us to set up a discovery call.









