The current flu season isn’t over yet but is already on record as the worst seen in nearly a decade. Here is a recap of the season so far and three key takeaways from the 2017-18 flu season.
The Flu in Review: What We’ve Seen to Date During the 2017-18 Season
Based on the reported flu levels from Center for Disease Control and Prevention (CDC), this season will go down as the worst since the 2009-10 “swine flu” season. In fact, the emergence of the H3N2 flu strain this season has proven especially difficult to fight and has been even more fatal. Bolstered by a heavy flu season in Australia and the hurricanes in the Gulf that cut into the availability of I.V. bag and fluid supply, the total impact to date in the U.S. has been significant:
- Over 217,000 hospitalizations due to flu-like symptoms, ending February 24 (CNN)
- Highest rate of laboratory-confirmed influenza hospitalizations in the past 10 years with 86.3 cases per 100,000 people (CDC)
- Hospitals operating at max capacity, and in many cases exceeded capacity as well as staff and equipment shortages (Time)
- Pneumonia and influenza-related mortality rates have exceeded epidemic thresholds (CDC)
And the flu season still has several weeks to go.
In January, the CDC estimated that flu cases had peaked between Christmas and New Years Day, but cases continued to rise throughout January and into early February. Although the flu appears to be subsiding rapidly now, patient census remains high. In fact, over a nine-week period during the current flu season, the percentage of influenza-related hospitalizations were equal to, or higher than, the highest peak in the 2016-17 season for percent of visits for influenza-like illness (ILI). As a result of this season’s severity, many hospitals are already trying to predict and prepare for next year.
Looking ahead, influenza experts say there is a high chance of a new flu pandemic emerging in the coming years. With an inevitable flu season every year, hospitals must identify how they will meet the pending demand and avoid finding themselves under-prepared. Especially with experts indicating that, as a nation, the U.S. is less prepared today for a major outbreak than we were for the H1N1 strain.
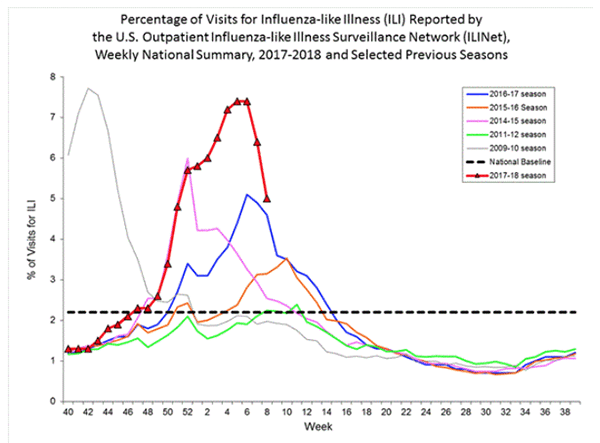 |
| *Source: CDC |
High flu rates and the lack of preparedness come at a cost. The CDC reports that the flu costs the U.S. $10.4 billion annually in direct medical expenses. It also marks several months where hospitals find themselves short on hospital beds, critical medical equipment, and other supplies as they scramble to manage a higher influx of census. Without the right resources and a plan in place ahead of the flu season, many hospitals experience shortages, a spike in supply chain-related costs, and a higher burden on their clinical engineering teams.
Looking Ahead: How Hospitals Can Prepare for the Next Flu Season
Leading up to the 2017-18 flu season, Agiliti shared an article offering three tips to consider while preparing your equipment inventory for the flu season. These tips remain applicable today, tomorrow, and in the coming 2018-19 flu season as well:
-
- Reduce equipment repair and maintenance backlogs
Infusion pumps and ventilators that are overdue for PMs or are in need of repair during the flu season can result in equipment availability issues, excess rental costs due to downtime, and ultimately increase nurse and patient dissatisfaction. Hospitals can mitigate challenges and unnecessary costs by reducing repair and maintenance backlogs in advance of a census spike. - Ensure rental equipment is maintained to high-quality standards
Don’t sacrifice patient safety and regulatory compliance in the pursuit of needed medical equipment. Instead, any time you need to rent medical equipment, dive into your provider’s cleaning and maintenance process. Ensure they are ISO 13485 compliant. And ask these 7 key questions about the quality of their rental equipment. - Secure high-use, critical rental equipment early
The flu season drives increased rental demand for respiratory equipment, hospital beds, and therapy surfaces. During a severe flu season, patient demand can outpace both providers and hospitals alike, leaving staff members to call around in search of the right device. Cut the risk and secure a flexible agreement for the critical equipment you need during the busy months. Not only can it guarantee access, but it can also reduce the wear and tear on your devices.
- Reduce equipment repair and maintenance backlogs
Please contact Agiliti if you would like to learn more about the steps you can take to get prepared for the remainder of this flu season or the start of next season. You can also visit our Resource Center to learn more.










