Background
Severe obesity prevalence (BMI of 40 or greater) has doubled within the United States over the past 10 years—from 4.7% to 9.2%.¹ As this trend continues, an increased strain is placed on the healthcare system, specifically hospital staff tasked with mobilizing these individuals. According to the Facility Guidelines Institute’s (FGI) definitions, an individual of size is considered anyone overweight by more than 100 lb., a body weight greater than 300 lb., or a body mass index (BMI) greater than 40.² While this is a good representation for an individual of size, no criteria exist to differentiate individuals who are much larger than this threshold. Patients over 700 lb. and over 100 BMI are under-represented in the literature and provide significant safe patient handling challenges to the care team.
Methods
Clinical case analysis is based on the following: patient is a 40-year-old male admitted to the hospital for worsening shortness of breath and edema secondary to chronic diastolic heart failure. He is 5’ 10” and upon admission weighed 865 lb. with a BMI of 124.
Phase One of therapy was focused on improving bed mobility and sitting tolerance. The ceiling lift and 3-to-4-person assist was utilized to get the patient sitting edge of bed (EOB). Phase Two focused on improving frequency and length of sitting trials, seated therapeutic exercise, and trunk control. The bariatric stretcher chair was utilized throughout this second phase. The patient transferred to the bariatric stretcher chair with the use of a ceiling lift. In the chair position the patient performed sitting tolerance, dynamic trunk control and seated exercises. When the patient became fatigued, he could rest in a reclined position using the tilt-in-space feature. Once sitting tolerance improved, weightbearing was introduced. The third phase consisted of weightbearing progressions, standing tolerance, and functional transfers. The stand-assist feature of the bariatric stretcher chair helped gradually increase weightbearing from ~0% to ~25%. At this point, he was able to perform a supine-to-sit transfer with minimum assistance and use of bed trapeze. The therapy staff then utilized the powered sit-to-stand lift to perform standing trials, which slowly progressed in length. After he gained confidence with standing, the patient progressed to functional transfer training with the use of two canes.

Findings
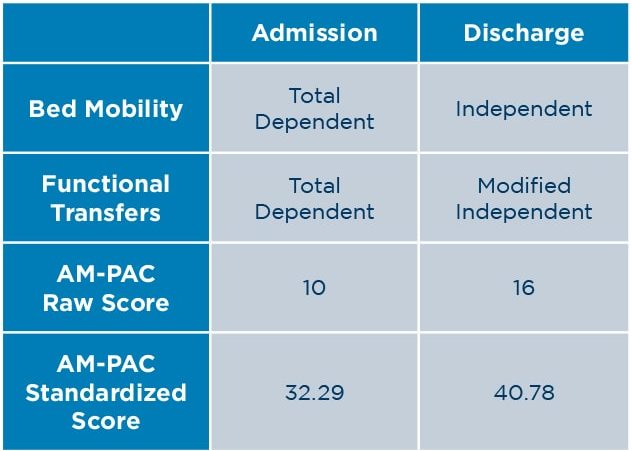
Over the course of his hospital stay, this patient’s bed mobility improved from total dependent to independent and his functional transfers improved from total dependent to modified independent. The Activity Measure for Post-Acute Care (AM-PAC) Basic Mobility Inpatient Short Form was used to assess the patient’s mobility levels. AM-PAC raw scores were converted to AM-PAC standardized t-scale scores for data analysis using a conversion table.³ His AM-PAC raw score increased from 10 to 16 and his standardized score from 32.29 to 40.78. According to Hoyer et. al., the Minimal Detectable Change at 95% Confidence Interval (MDC95) for the AM-PAC Basic Mobility standardized score is 4.49.4 This patient’s improvement of 8.49 was well above the 4.49 MDC95 threshold.
Conclusion
After seven months of hard work by the patient and staff, he was able to return home. Specialty equipment was a vital piece of the patient’s progress and important for keeping staff safe. Throughout the course of care, staff utilized a 48” wide bed frame with trapeze, ceiling lift with XXL hammock sling, bariatric stretcher chair,5 and powered sit-to-stand lift. This equipment helped facilitate safe and timely mobility of this patient, while keeping hospital staff safe from injury.

