Purpose
The purpose of the project was to identify and develop guidelines for multiple uses of powered low air loss (LAL) within the neonatal and pediatric population at a Magnet Designated Children’s Hospital.
Background
Diaper dermatitis is one of the most common dermatological diagnoses in the neonatal and pediatric population. Diaper dermatitis has been identified in 25% of the general diaper-wearing pediatric population. Alteration in skin integrity can cause physical pain and suffering to the child and mental anguish to the parents. Depending on the severity of the dermatitis and disruption in the skin, increased length of stay and additional financial expense may result.
Objectives
Based on the algorithm outcomes, determination was made if a powered LAL pediatric crib surface was appropriate for integration into the care plan. The CWON and FNP-C led the guideline development initiative with (1) identification of at-risk patients, who would benefit from an alternative support surface, (2) development of guidelines to provide moisture management in the neonatal and pediatric patient population, and (3) development of a patient algorithm to assess the patients’ Braden Q or Neonatal Skin Condition Score and Neonatal Abstinence Score (NAS).
10-Month-Old Male

Post Operative Day: 9
DTI, 9 cm x 3 cm x unknown depth, Etiology: neonatal positioning device
Treatment Plan:
- Powered low air loss: pulsation mode
- Cycle time: 3 minutes
- Silver foam dressing

Post Operative Day: 29
DTI, 4.5 cm x 0.8 cm x unknown depth

Post Operative Day: 34 (Resolved DTI)
Patient remained hospitalized for an additional 117 days on the powered low air loss mattress. No additional pressure ulcer development.
4-Month-Old Female

Day of life: 117
Severe perianal dermatitis
Treatment Plan:
- Powered low air loss: pulsation mode
- Ph-neutral soap and saline
- Hydrophilic cream

Day of Life: 153
Area Improved Visible Scarring 0.75 cm x 0.75 cm
3-Week-Old Female

Day of Life: 21
Severe perianal dermatitis
Treatment Plan:
- Powered low air loss: pulsation mode
Cycle time: 3 minutes - Ph-neutral soap and saline
- Hydrophilic cream
- Turn every two hours

Day of Life: 29
Treatment Plan:
- Patient discharged to home
- Continue Ph-neutral soap and saline
- Hydrophilic cream with each diaper change
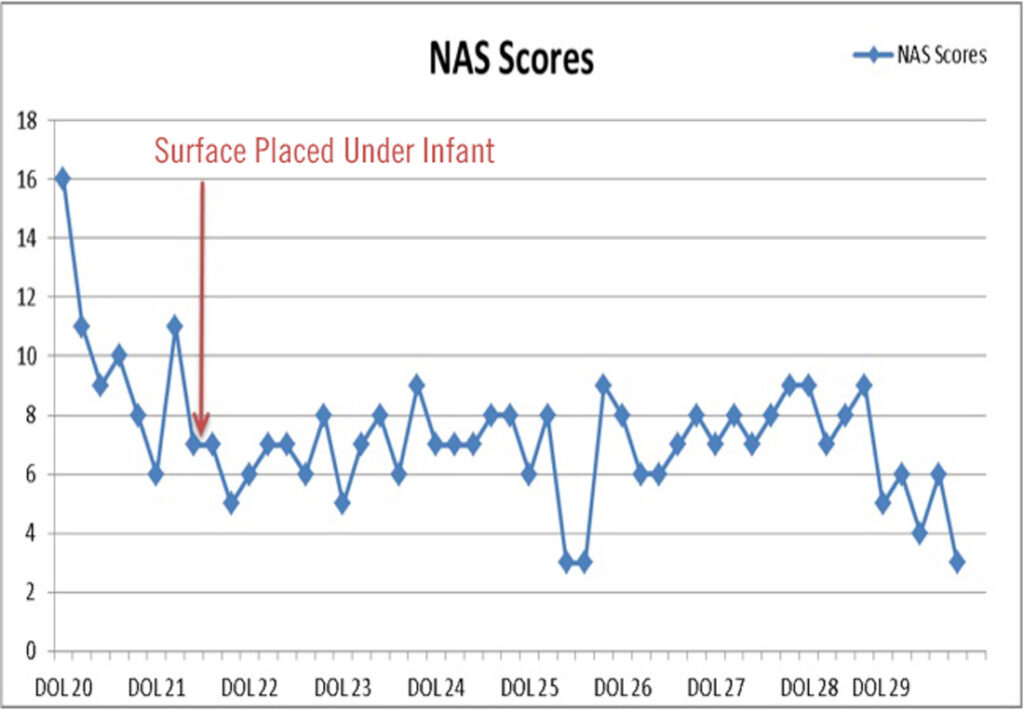
NAS Impact
Morphine began day of life 3; stabilization dose of 0.05 mg/kg. Morphine prescribed dose 0.4 mg/ml; frequency taper q3 to q12 hours; complete by day of discharge. Perianal dermatitis resolved in 8 days with initiation of powered low air loss mattress system and adjunctive treatment plan.
Discussion
Integration of the powered LAL pediatric surface was successful with guideline development for primary services that are able to identify at-risk patients and early therapy initiation. Use of the powered LAL pediatric crib surface has steadily increased since inception.
Patients with diagnosed moisture-associated diaper dermatitis demonstrated improved healing times of one week upon initiation of powered LAL therapy. A powered LAL surface has shown to be effective in interrupting the cycle of contributory events leading to diaper dermatitis.
Improved sleep pattern along with a decrease in NAS (from 11-14 to 5-8) have been associated with the integration of powered LAL for patients diagnosed with Neonatal Abstinence Syndrome.

