The previous two flu seasons were notable for two distinct reasons. Neither of which were positive. But both seasons do provide healthcare facilities with important lessons to be learned.
Like it or not, now is the time to start preparing for the flu season — making sure your facility is ready to do all it can to prepare for increased patient acuity and census before the flu rears its ugly head. To prepare for what’s ahead, let’s start by looking back.
Looking back: The worst — and longest — flu seasons in a decade
If you think the last two flu seasons were more intense, you’re right. According to the CDC, the 2017-18 flu season was the deadliest in more than four decades, and the first on record to be classified as high severity in all age categories.
From October 2017 to April 2018, an estimated 48.8 million individuals in the U.S. came down with the flu, with 959,000 hospitalizations over that period. Sadly, the U.S. Surgeon General estimated that 80,000 Americans died during 2017-2018 season due to complications resulting from the flu.
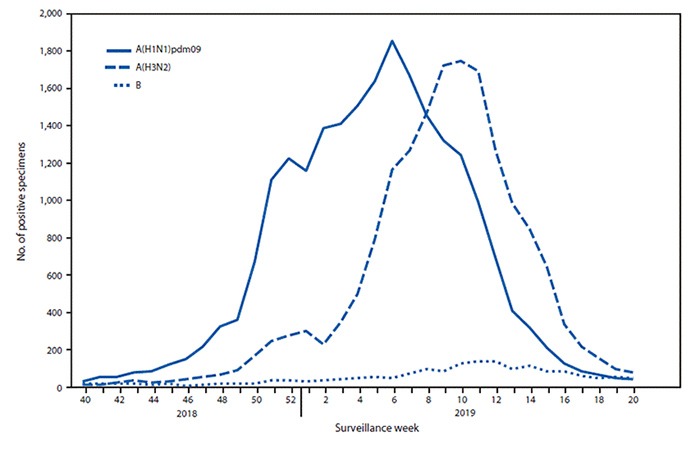
Following the deadliest flu season in a decade, the 2018-19 flu season turned into the longest season over the same time frame. The 2018-19 flu season officially lasted 21 weeks, during which the CDC estimated that 42.9 million people got sick, with around 647,000 people hospitalized — and more than 20,000 deaths documented as a result of complications from the flu.
The emergence of a “second wave,” which included a second, tougher strain of the flu, was particularly devastating last year and extended the season beyond the typical timeframe. While the 2018-2019 flu shot had been performing above average through February, the CDC says the vaccine provided “no significant protection” against the second wave. This led to a spike in hospitalizations and dragged the flu season late into the spring.
Looking forward: A better vaccine — with potential delays
The devastating “second wave” of the last flu season led the FDA’s Vaccines and Related Biological Products Advisory Committee (VRBPAC) and the World Health Organization (WHO) to take the rare step of delaying the decision on which influenza strains to include in the 2019-20 vaccine. This vaccine was finalized in May — two months later than usual — giving researchers needed time to study the late-emerging flu strain from last season. Experts say this delay will increase the likelihood of a vaccine “match.” In other words, there’s a better chance that this year’s flu shot will stop the most common strains of flu for the coming season.
However, the delay in finalizing the vaccine composition also delayed production of the more than 162 million doses of vaccine required to protect the global population. The CDC is currently recommending that healthcare providers and pharmacies prepare for a two to four week delay in vaccine availability.
Tips for getting ahead of the flu frenzy for your facility
The potential delays in availability of this year’s flu vaccine mean that hospitals and care facilities need to focus on building up their other defenses against the introduction and spread of the flu within their facilities. Perhaps more than ever, it’s critical to take early and added precautions to ensure your facility is prepared for flu season.
Here are some essentials steps you can begin taking now in order to protect your facility and your patients against the flu:
- Take time to debrief with impacted department stakeholders on last year’s flu season
Different departments will provide different perspectives on how last year’s flu season affected them and the hospital. Meet with a cross-functional team from supply chain, nursing, respiratory, pharmacy, biomed and other select stakeholders to discuss lessons learned and what to do differently this year. Determine if there were equipment or supply shortages, service request backlogs, staffing shortages, etc. Were nurses and therapists able to quickly access medical equipment when it was needed? Engaging multiple stakeholders across departments yields better line of sight into true equipment demand and availability, which can help inform equipment purchasing and rental decisions for the upcoming season. - Reduce medical equipment repair and maintenance backlogs
You can’t always plan ahead for staffing shortages. Whether you’ve got open positions in your clinical engineering department or team members on military leave, being short-staffed can result in critical equipment – like infusion pumps and ventilators – to be past-due on PMs or create a backlog of repair. During the flu season, this delay can be exacerbated, causing equipment availability issues and unnecessary rental costs due to equipment unavailability. In the end, this can lead to lower patient and nursing satisfaction. Hospitals can mitigate challenges and unnecessary costs by reducing repair and maintenance backlogs in advance of a census spike. - Start planning NOW for your critical rental equipment needs
It’s never too early to start preparing for the flu season. Why? Because flu season drives increased rental demand for certain types of equipment, like respiratory, infusion pumps, beds and therapy surfaces. During a severe flu season, census demand can surpass both providers and hospitals alike, leaving staff members to scramble and call around in search of the right equipment. Get ahead of the demand by securing a longer-term flexible agreement early for the critical equipment you need during your busiest months. Not only does this guarantee equipment availability, it reduces the wear and tear on your owned devices so they last longer. - Keep patient safety top of mind with rental equipment maintained to high-quality standards
Patient safety is one of your facility’s top priorities. Don’t sacrifice it by using vendors you haven’t fully vetted for adhering to important regulatory standards and that prioritize patient safety. Any time you need to rent medical equipment, know what questions to ask and dig into your rental provider’s cleaning, maintenance and biomedical training processes. Ensure they are ISO 13485:2016 compliant. And ask these 7 key questions about the quality of their rental equipment. - Optimize your equipment usage (and don’t over purchase)
During the capital planning process, most hospitals choose to purchase based on their maximum census level to ensure that they have more than enough equipment for a high influx of patients (flu season). The trouble is, maintaining this inventory level comes with additional service costs and a higher burden on both the nursing and biomed teams to manage. In fact, the average utilization for medical equipment is around 42% – due to a variety of departmental process breakdowns. Before purchasing more equipment, conduct an inventory review and identify common gaps between departments that prevent equipment from being readily available. You can also establish an ideal owned-to-rented equipment mix that can help you get through the busy months without spending unnecessary capital.
Don’t wait for the chill in the air to remind you about flu season. Agiliti can help you start taking simple steps today to get prepared for next flu season. Depending on your facility, this could include:
- A high-level review of your current inventory to establish an ideal rent-to-own equipment mix
- Supplemental biomedical repair and maintenance services
- Long-term rental agreements for high-use movable medical equipment
Contact your Agiliti rep to learn more.
You can also visit our Resource Center to learn more.











